Why antibody levels do not equal "immunity": Part 2
Epithelial cells and mucus!
We constantly hear about antibodies in the context of “immunity.” In fact, this is how the CDC defines “immunity”:
Immunity to a disease is achieved through the presence of antibodies to that disease in a person’s system.
In Part 1, we saw how this was grossly misleading, because it’s possible to recover from SARS-CoV-2 infection without the help of antibodies in the blood. This obviously means that there are other components of the immune system that are relevant to fighting off viruses like SARS-CoV-2.
In this article, we’ll review two underappreciated components of the immune system: the epithelial cells that form the barrier of our respiratory tract, and mucus.
In future articles of this series, we’ll review other components of the immune system.
This background knowledge of the immune system will allows us to compare “natural immunity” with the immune response provoked by the COVID-19 vaccines.
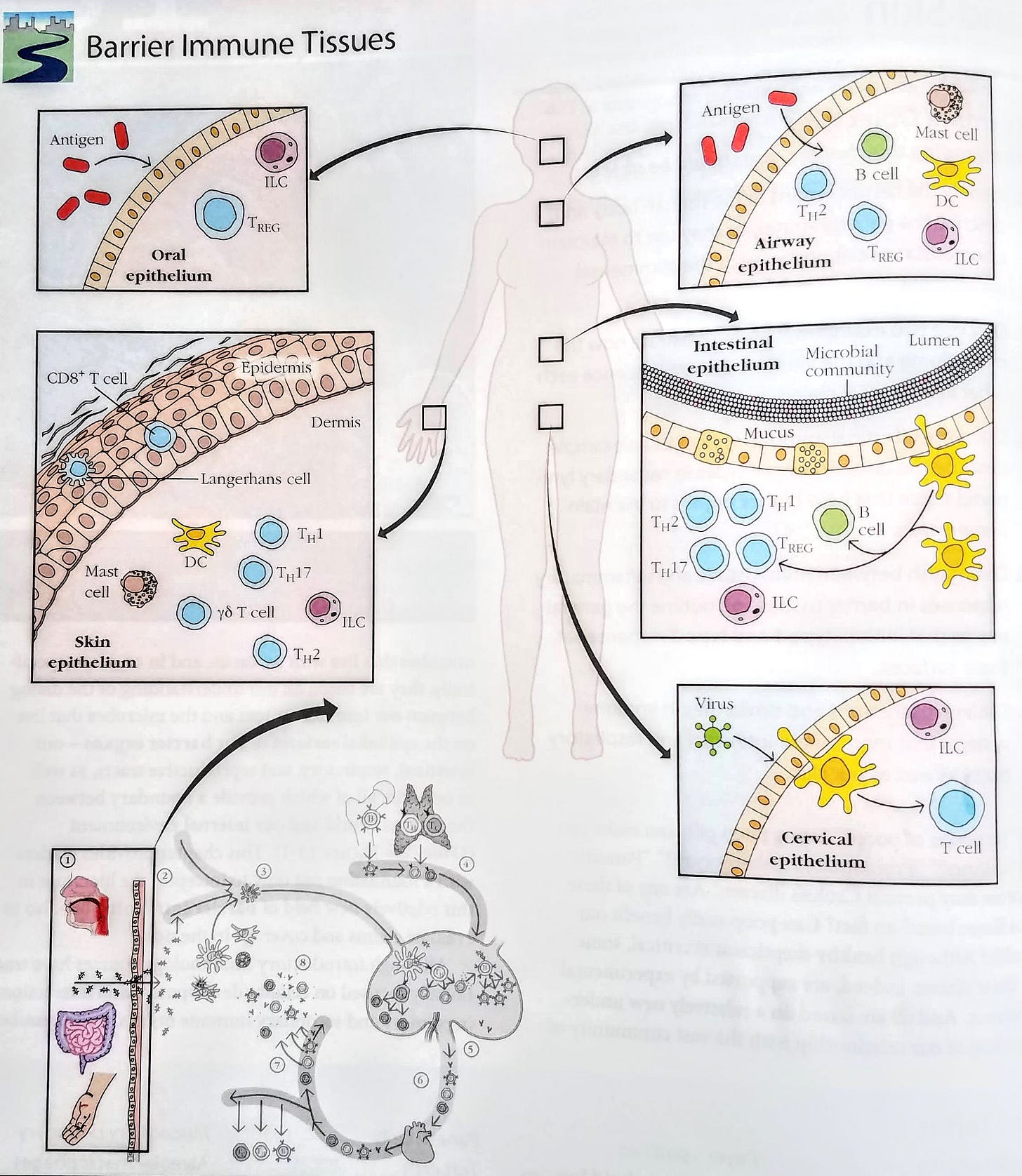
The cells at our barriers
The outer layer of the body’s surface is made of epithelial cells. These cells cover any part of the body that comes into contact with the “outside” world; this includes the skin, airways, gut, and urinary tracts.1
Mucus
Specialized epithelial cells secrete mucus, which is viscous and gel-like. The image below shows a layer of epithelial cells with a layer of mucus on top:
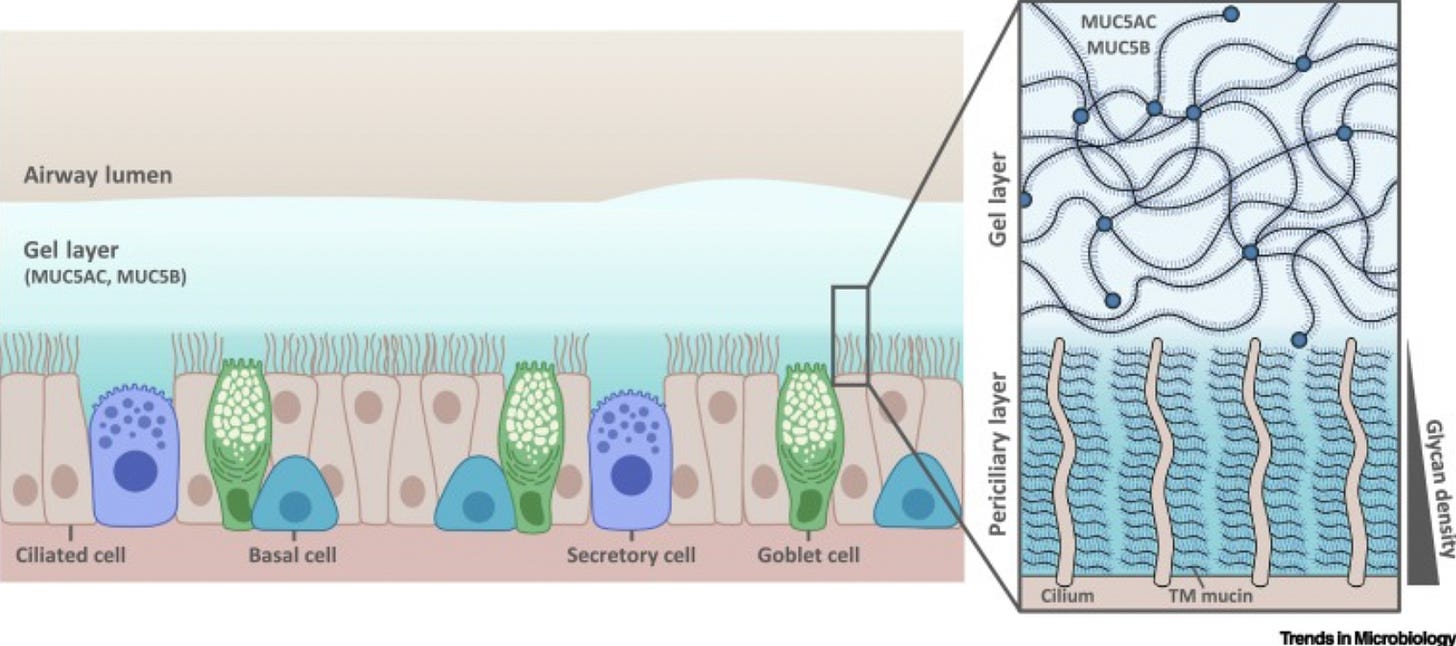
The mucus forms a mesh-like layer which acts as a “sieve” for pathogens. This can trap pathogens that are larger than the pore size of the “sieve.”
Mucus contains several different types of molecules called “mucins.” These are large molecules with lots of different carbohydrate chains. The chains offer a high degree of resistance to enzymatic breakdown from microbes.
In order to learn what these different mucins do, researchers have created mouse strains that lack a gene for one of the mucins.
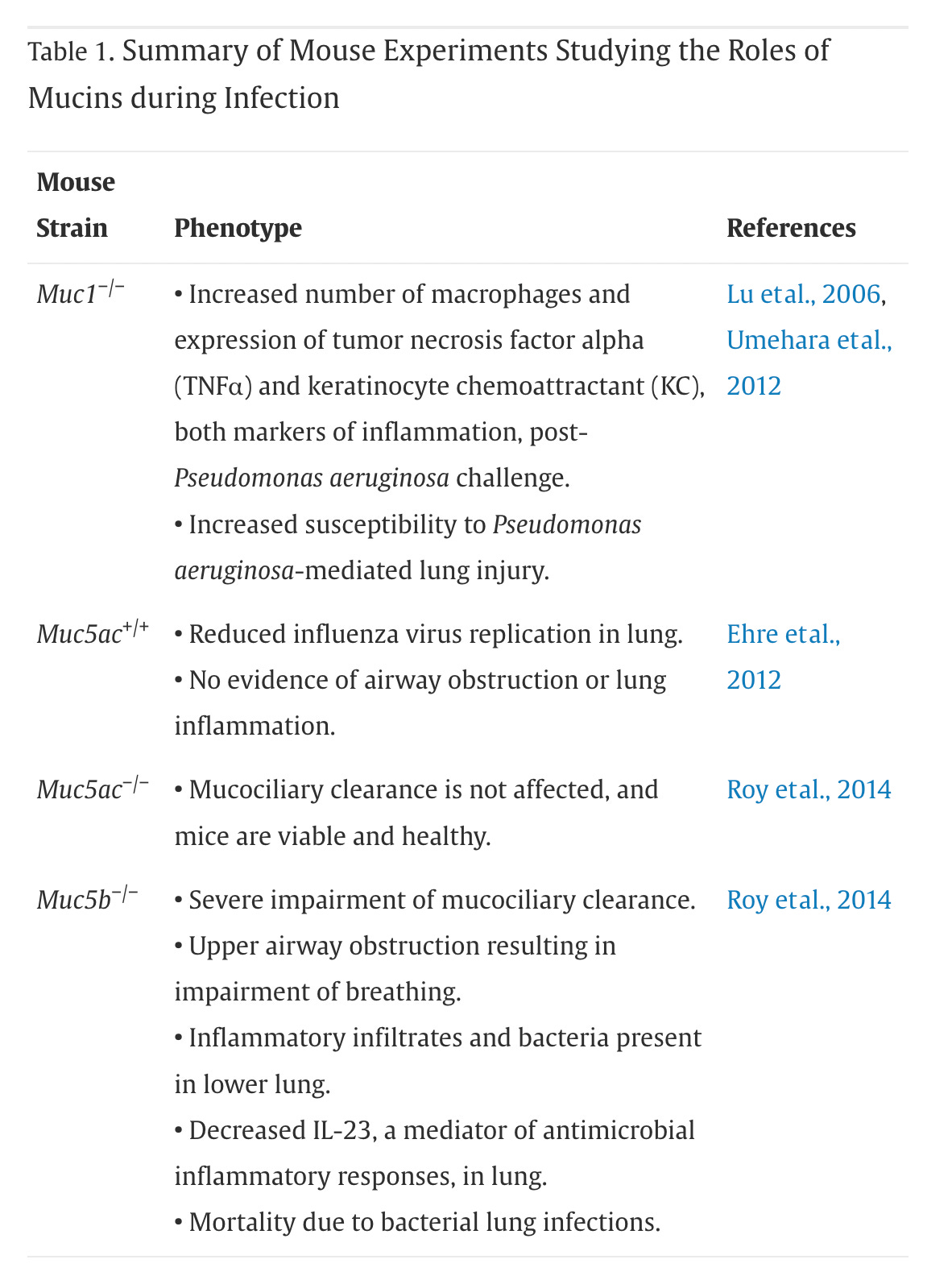
These experiments revealed, among other things, that a mucin called MUC5B is particularly important for normal airway function. Mice that lack the ability to make this mucin are much more susceptible to infections in the lungs.
Molecules in mucus can act as “receptor decoys” for viruses. Normally viruses need to bind to receptors on the surface of cells in order to infect them, but “receptor decoys” can bind certain viruses and help trap them (more here).
Mucus also contains numerous other compounds involved in defense. These are just some of them:
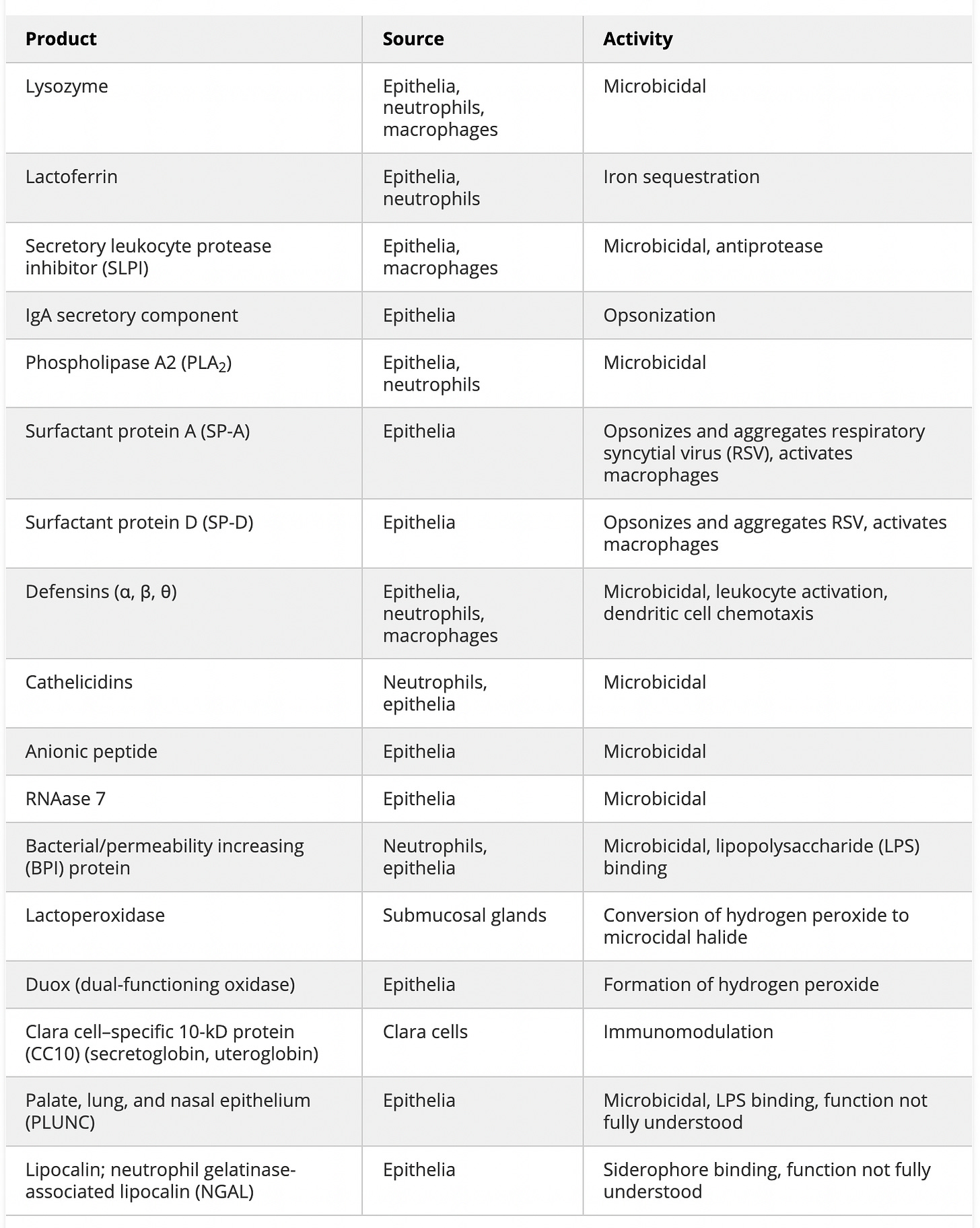
You’ll see quite a few microbicidals on the list, which are compounds that kill microbes like bacteria or viruses.
Some of these, like surfactant proteins, work as “opsonizers,” which tag foreign proteins for elimination by immune cells. Then there’s lactoferrin, which sequesters iron, making this nutrient unavailable to bacteria. Lactoferrin also has antiviral properties, and may even have some efficacy against coronaviruses (more here).
Lysozyme, cathelicidin, and β-defensin work by perturbing the cell walls or membranes of pathogens. Defensins can be found in the serum (blood) as well. There’s some evidence that physical activity increases the production of serum defensins (more here and here).
There are many other mucosal antimicrobial compounds in mucus that aren’t listed here.
Epithelial cells play an active role in defense
Now let’s dig deeper into the epithelial cells that make up the barriers. The figure below depicts a simplified view of the cells that make up the airway epithelium:
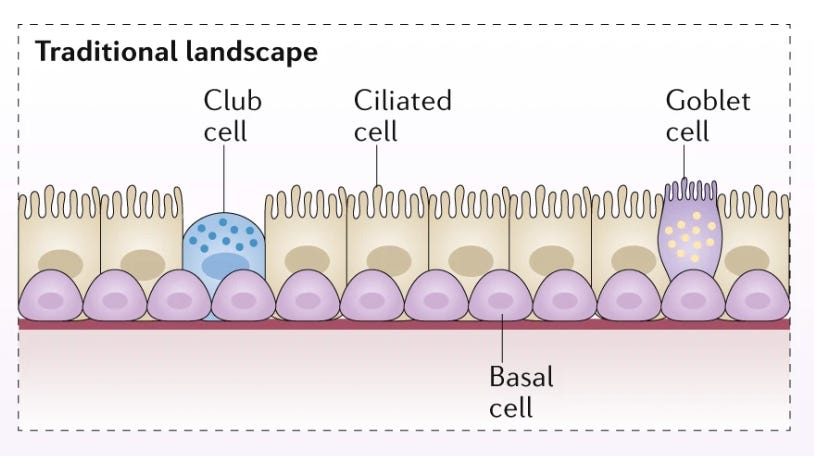
These cells not only form a barrier to the outside world, but also play an active role in defense.
Goblet cells secrete mucus, as well as immune signaling molecules (more here). Ciliated cells use their little hairs (cilia), to sweep mucus upwards to help expel trapped foreign particles or pathogens from the respiratory tract. Both basal and club cells can differentiate into other types of epithelial cells, and produce immune signaling molecules. Basal cells also produce antimicrobial molecules (see here).
More recently, we’ve learned of new cells types in the airway epithelium that are involved in immune defense. The image below shows a revised contemporary view that includes newly identified cell types:
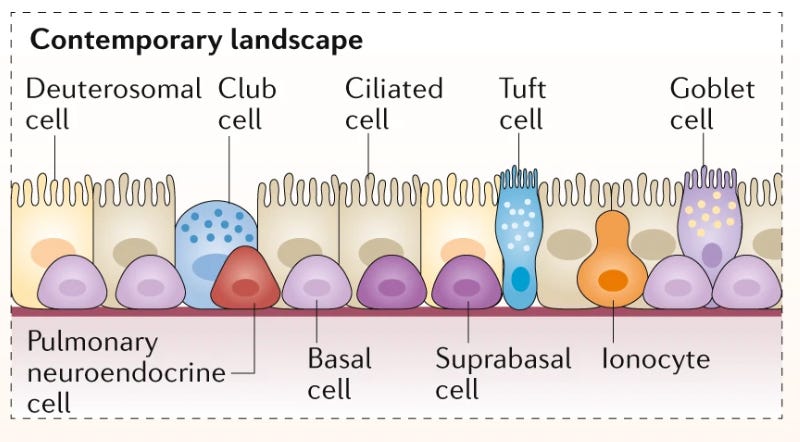
For example, tuft cells seem to be involved in promoting respiratory reflexes like sneezing. Their numbers expand following inhalation of common allergens. And pulmonary neuroendocrine cells are not well understood, but they seem to sense inhaled inputs in the airway and release neuropeptides that enable lungs to respond with mucosal immune responses (more here and here).
We’re also learning of new immune properties of airway epithelial cells:
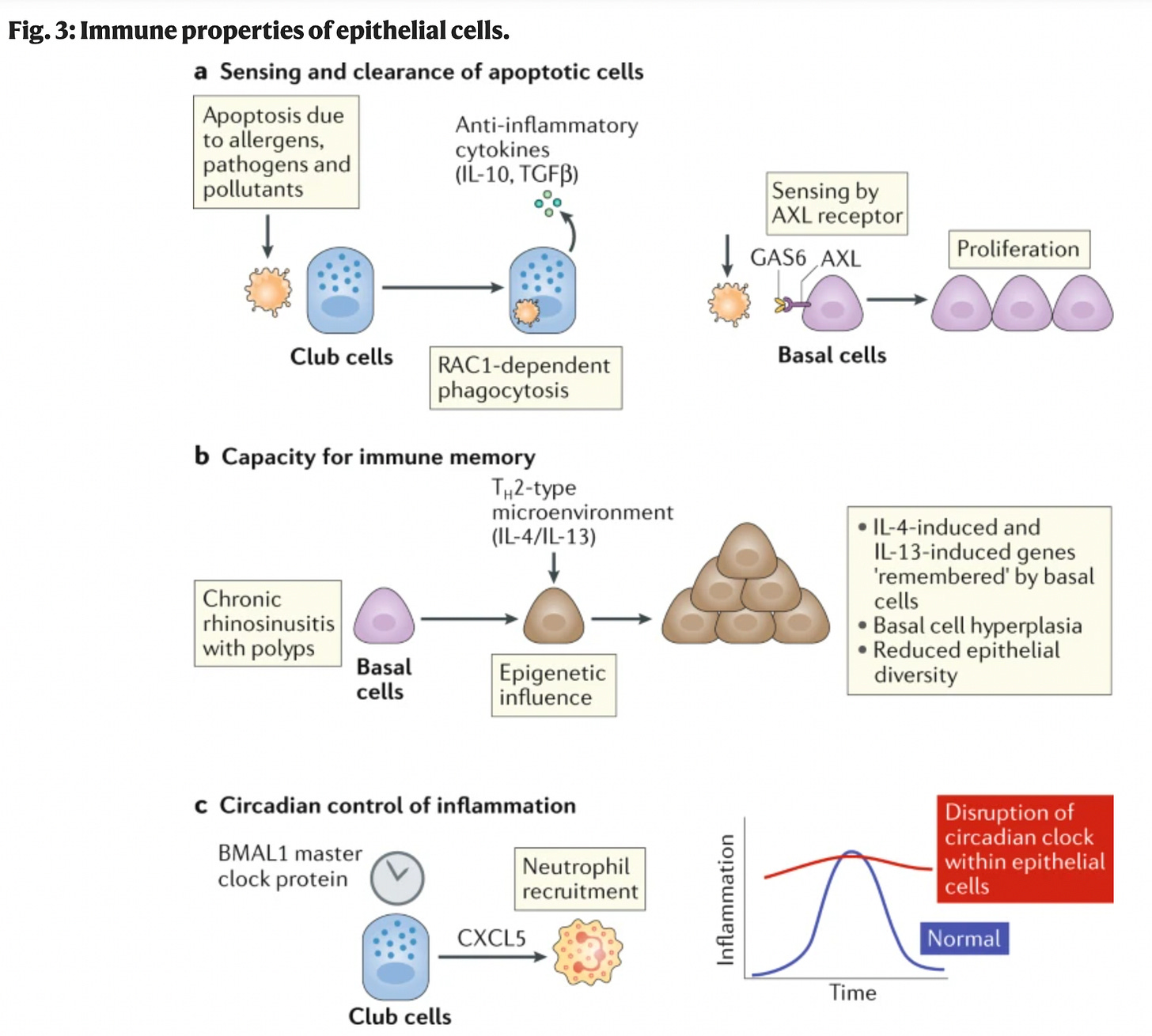
For example, in the presence of pathogens, or allergens, some cells in the airway will commit apoptosis, which is a form of cell suicide. “Textbook immunology” would tell you that these suicidal cells would get cleared by “professional” phagocytes, which are immune cells that engulf other cells. However, we now have evidence that certain airway epithelial cells also engulf apoptotic cells, and play a role in taming the inflammatory response (see Fig. 3a above).
We’ve also discovered that basal cells seem to have some capacity for “inflammatory memory” (more here, here, or here).2
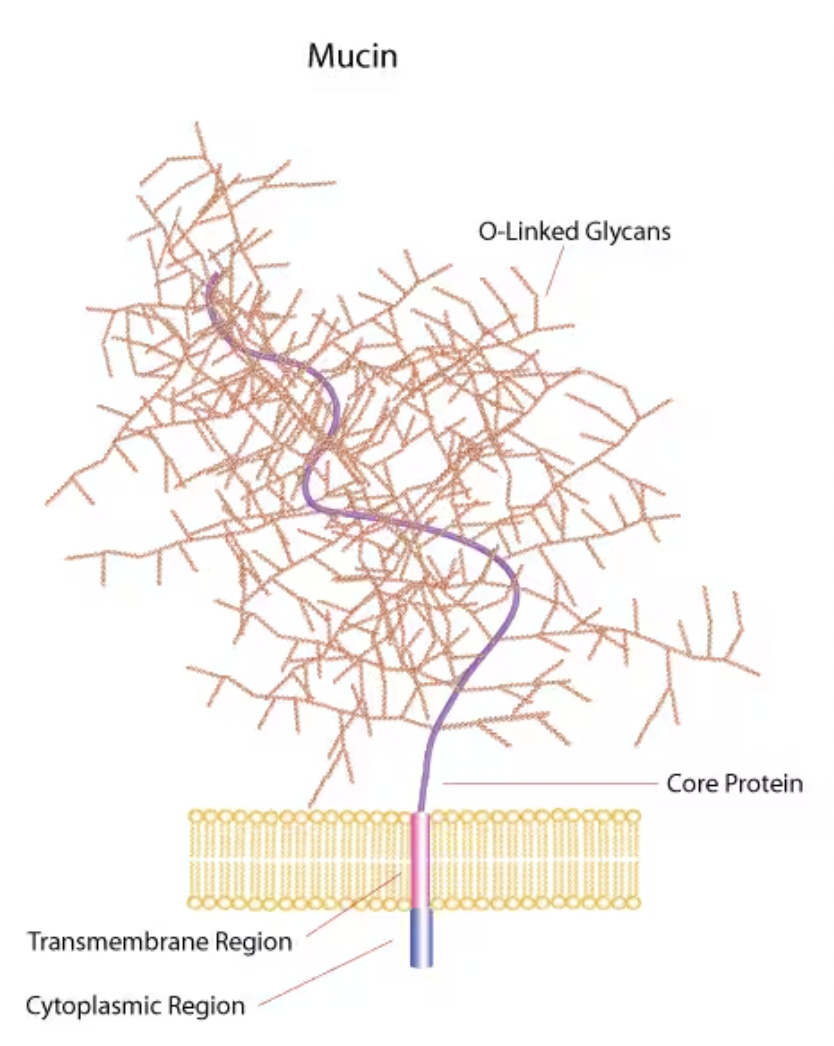
Epithelial cells modify and transport immune molecules
Epithelial cells also take immune molecules from below the mucosal layer, and transport them to the surface facing the airway.
For example, they transport antibodies like dimeric IgA (dIgA), which are made locally by antibody secreting cells (B cells) underneath the epithelial cell layer.
The image below shows this process:
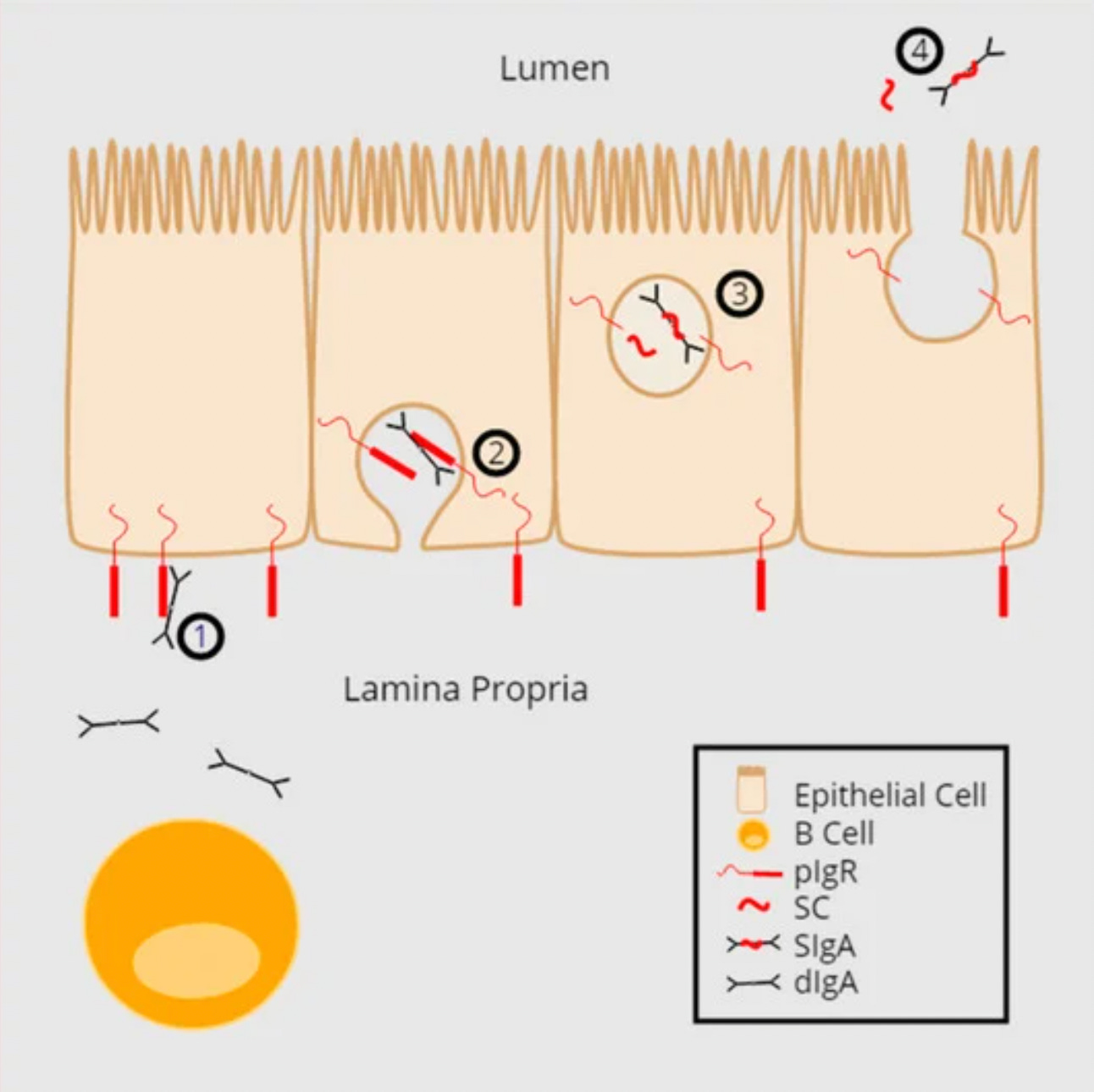
While they transport the dIgA antibody across the epithelial layer, something gets attached to it called “secretory component” (SC). The resultant molecule is called “secretory IgA,” or SigA.
Another type of antibody, IgM can also be transported this way, though the dominant class of antibody in the mucosal immune system is in the form of SigA. SigA can do many things, but one of its most important functions in the mucosa is to bind pathogens and block their ability to gain access to the epithelium (more here, here, and here).
By the way, IgA can also be found in serum (blood), but serum IgA is different from secretory IgA found in mucosa.3 One important difference is that secretory IgA usually leads to clearance of microbes in a way that's less inflammatory than the effect of serum IgA.
This makes sense because the mucosal barriers are constantly exposed to foreign particles and microbes; if the the body always reacted to these particles and microbes with a lot of inflammation, the barriers would be constantly inflamed.4
Selective permeability through the barrier
It should also be mentioned that there can be “seepage” from blood into the airway.
This flow of blood fluid through the epithelium not only flushes out invading pathogens, but also brings numerous plasma proteins to the mucosal layer. These include important components of the immune response, including serum antibodies and complement proteins (more here and here).
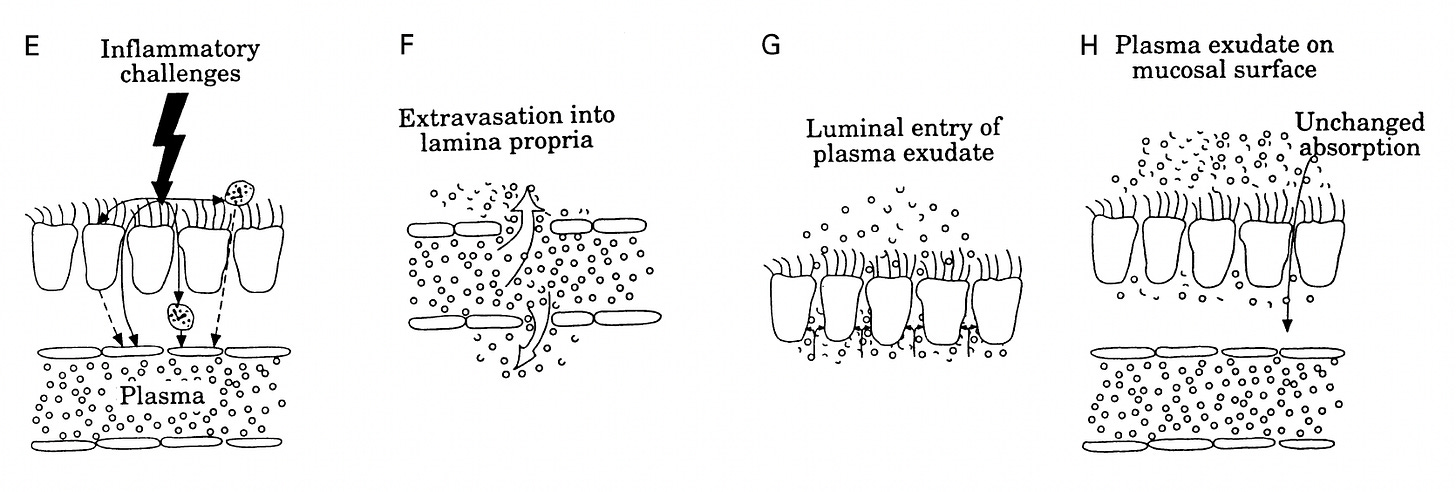
Under certain inflammatory conditions, chemical agents can be released that increase vascular permeability and allow even more blood fluids to seep through.
Epithelial cells relay information to immune cells
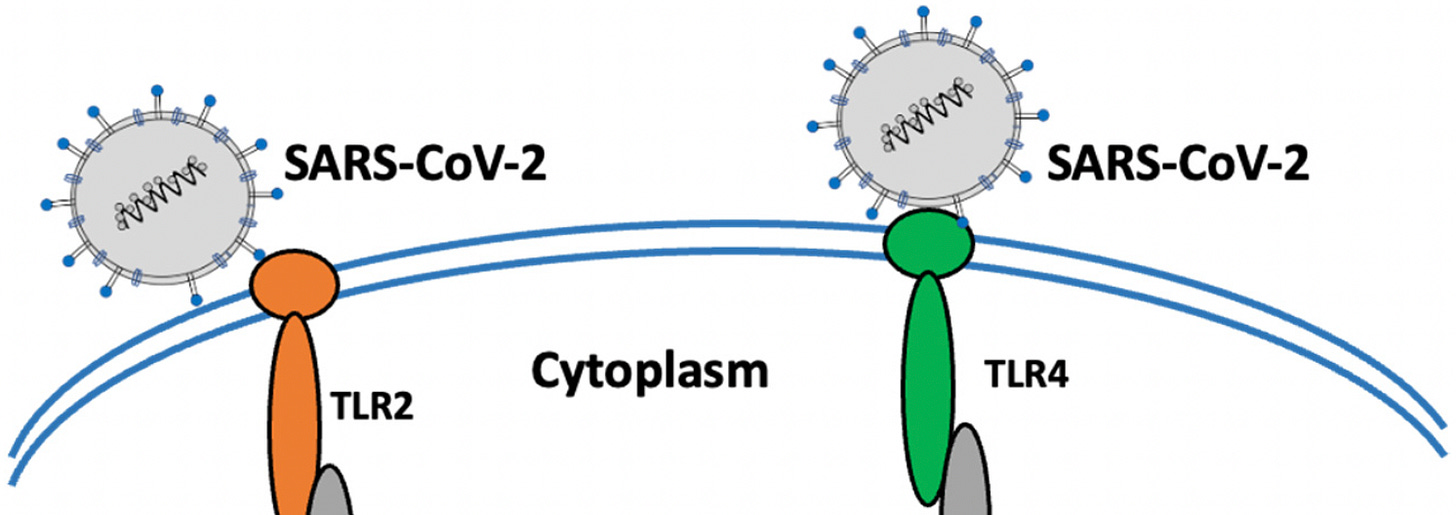
Since epithelial cells are at the barriers of the body, they are usually the initial targets of pathogens, and therefore serve as “sentinels” for infection. These cells have pattern recognition receptors (PRRs) that recognize patterns or motifs that are conserved across many bacteria and viruses.
Different receptors specialize in recognizing different patterns on pathogens. For example, mannose receptors specialize in picking up on sugars on the surface of pathogens. Toll-like receptors pick up on all different kinds of patterns on pathogens, including components of bacterial or fungal cells walls, or viral RNA.5
By the way, young people seem to express pattern recognition receptors at higher levels on their epithelial cells, compared to older people (see Fig. 2 here). Perhaps this is one reason why they generally manage SARS-CoV-2 infection well.
What happens if these receptors sense the presence of pathogenic microbes?
The epithelial cells release signals that alert other cells to the presence of pathogens, and recruit nearby immune cells.
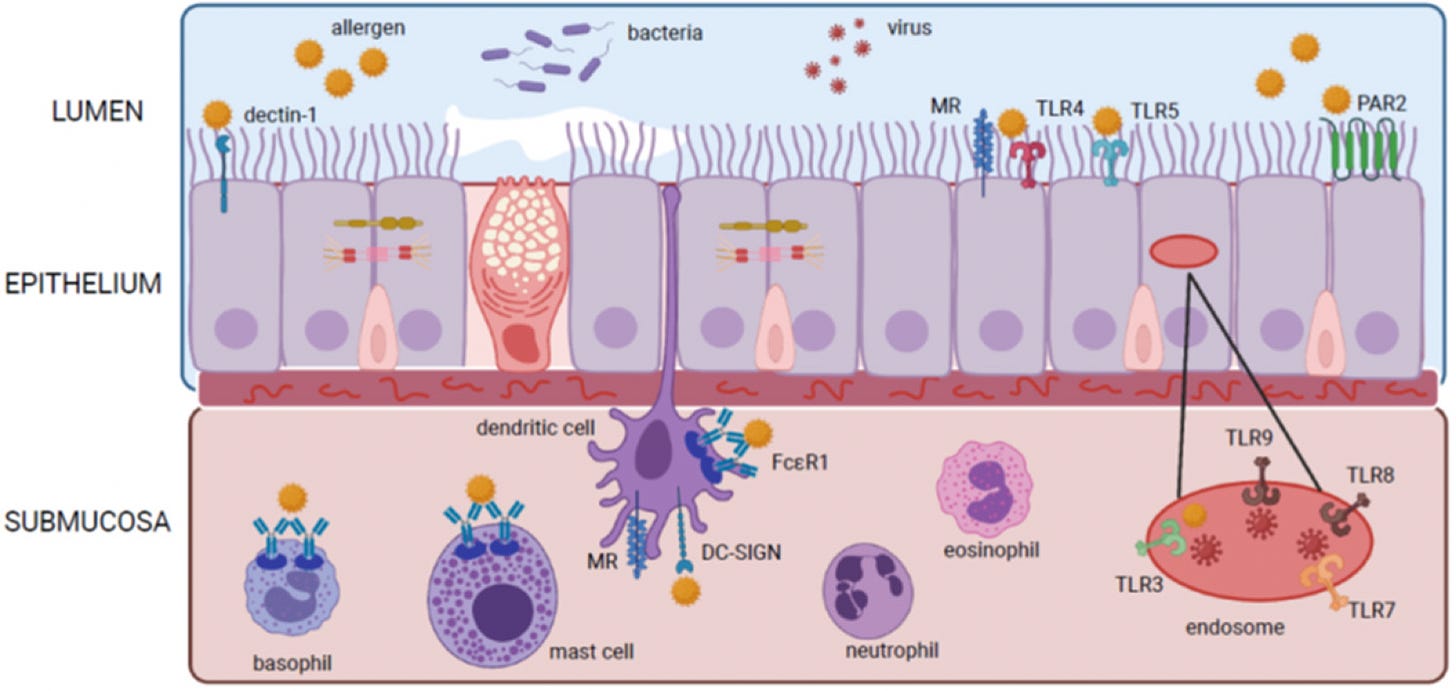
In the image above, some of those immune cells are shown below the layer epithelial cells.
In Part 3, we’ll talk about what those immune cells do.
By the way, in addition to our own cells there are commensal organisms that inhabit the airway; these are organisms like bacteria, fungi, etc. that aren’t necessarily bad or pathogenic. For a long time it was thought that these microbes only inhabited the upper airway, and the lower airway was believed to be sterile, at least in healthy individuals. Recently, however, there’s been evidence that healthy people also have microbes living in the lower airways. More here.
This “memory” is thought to come about from epigenetic changes in the cells, which is when DNA is reversibly modified to alter how genes are expressed without altering the underlying DNA sequence. This kind of “memory” is different from the kind of memory conferred as a result of “memory cells” that are part of the adaptive immune response (this will be discussed in more detail in future articles).
Whereas secretory IgA is dimeric, serum IgA is composed mainly of monomers, and also lacks the secretory component that secretory IgA has. This allows serum IgA to bind to certain receptors on myeloid cells. The net result is that serum IgA tends to induce more pro-inflammatory responses, compared to secretory IgA (more here).
This is a fascinating aspect of the mucosal immune system; how they maintain a balance between responding to pathogenic microbes, while not overreacting to harmless microbes. The way this is achieved is not completely understood.
Toll-like receptors (TLRs) can be found on the surface of cells, as well as inside of cells. TLRs that are inside of cells can pick up on viruses that have already gotten inside and infected a cell.

This is so cool. The immune system is one of the most amazing systems in the body. Thanks for explaining this.
Wow, unbelievable that the CDC is defining immunity in terms of antibodies. They are trying to rewrite biology and biological knowledge to help pharmaceutical companies sell products.
The human immune system is way more complex than anything Einstein came up with and it hasn't been completely figured out yet. 99% of the "experts" are clueless including many advanced scientists and doctors. But you don't have to understand everything. Here's a pro tip to those reading. If it ain't broke, don't fix it. My unfixed immune system has worked flawlessly these past three years. Zero problems/side effects/ worries. Great work as always.