In Part 1 of this series, we saw how the CDC defined “immunity”:
Immunity to a disease is achieved through the presence of antibodies to that disease in a person’s system.’
In that article, we went over why this definition was grossly misleading, because there are many other components of the immune system that are relevant to fighting off infections, besides antibodies.
This article is part of a series that reviews the other components of the immune system. In this article, we’ll focus on what’s called the “innate” immune system. This part of the immune system gets much less attention in the media compared to antibodies.
Innate immunity
The immune system is usually divided into two branches: the “innate” and “adaptive” immune systems. Mucus and epithelial (barrier) cells, as discussed in Part 2, are part of the innate immune system.
The innate immune system is the first line of defense against pathogens. Cells of the innate immune system,1 as mentioned in Part 2, have receptors on or inside them, that recognize general patterns of bacteria, fungi, and viruses.2 These are partially what allow them to rapidly recognize pathogens and respond to them on the order of minutes after exposure.
The table below shows some of these receptors and the types of molecules (ligands) they recognize:

Cells of the adaptive immune system usually take longer to come on board because they’re more attuned to subtle molecular differences (to be discussed in Part 4 of this series).
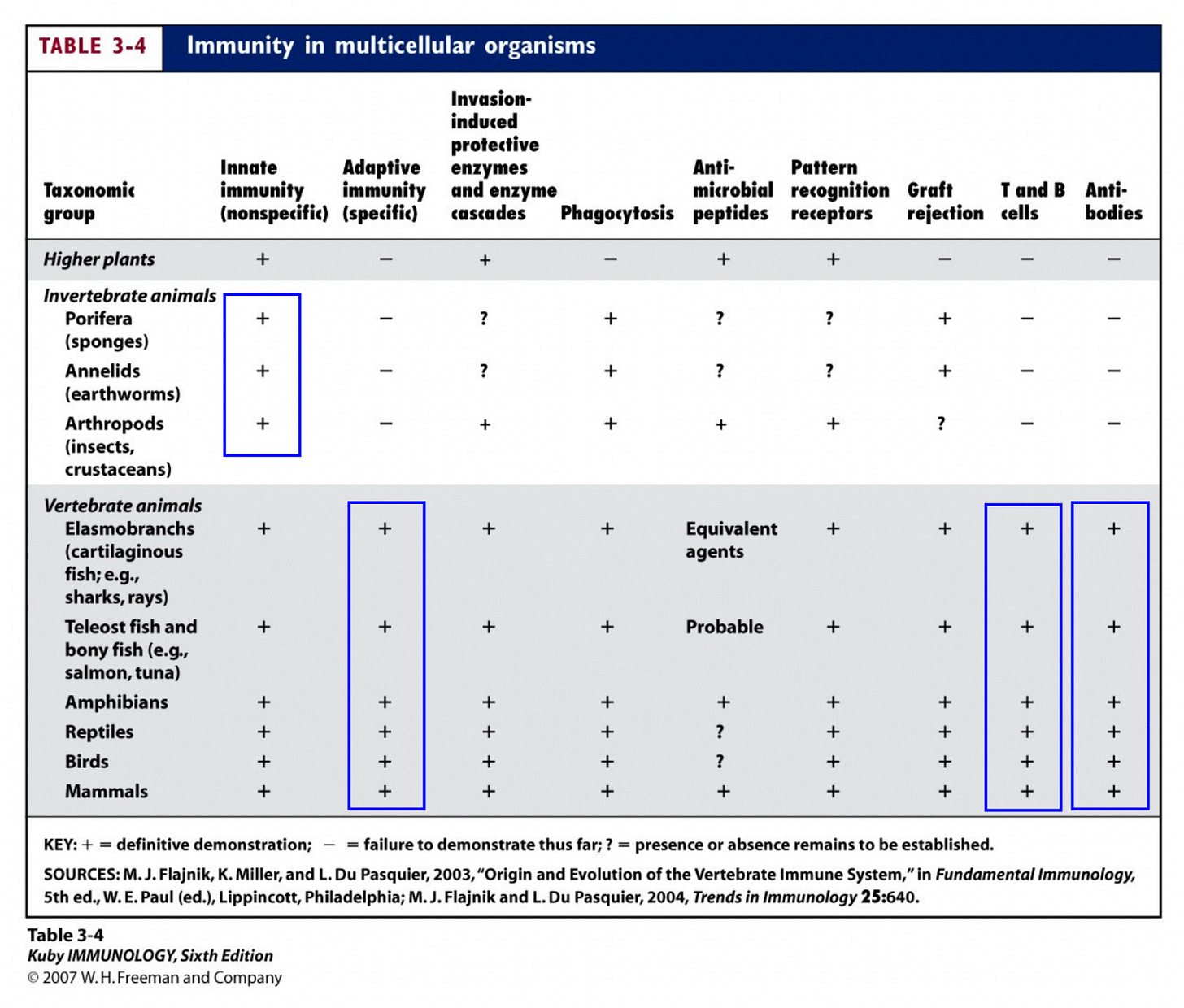
Innate immunity is usually described as more “primitive” than adaptive immunity. Innate immunity is found among all multicellular organisms, whereas adaptive immunity is only found among vertebrates.
Despite the fact that the innate immune system is “primitive,” it’s highly complex, and there’s still a lot we don’t know about it. Our understanding of the innate immune system is continually evolving, and this article will attempt to incorporate some recent research on innate immunity, including information that isn’t generally found in immunology textbooks.
Overview of the cells of the immune system
The image below shows the cells of the immune system, and where they’re derived from. All the cells of the immune system are derived from what’s called a “hematopoietic stem cell,” which is a type of immature cell that can differentiate into different types of cells of the immune system.

All the cells that are blue or green are part of the adaptive immune system, with the exception of natural killer cells. The cells that are pink and purple, as well as natural killer cells, are considered part of the innate immune system.
Sometimes you’ll see references to “leukocytes” or “white blood cells”; these refer to all the cells of the immune system pictured above except red blood cells. Red blood cells aren’t generally considered part of the “immune system,” though there’s been some recent work to suggest that they play an important role in innate immunity.3
Next, we’ll do a quick overview of the different types of cells that are part of the innate immune system.
Granulocytes
“Granulocytes” include the following four types of white blood cells: neutrophils, eosinophils, basophils, and mast cells. In the image below, they’re the ones circled in red:
Granulocytes are named after the membrane-bound granules (sacs) they contain, which hold toxic proteins that can be used to kill pathogens.
Neutrophils
After red blood cells, the most abundant cells in the blood are neutrophils. Neutrophils are often said to make up the first wave of cells that cross blood vessel walls to enter into infected or inflamed tissue.4
Near sites of inflammation, blood vessels get dilated (widen), which causes blood flow to slow down in the area, allowing white blood cells to linger and interact with the inner walls of the blood vessels. Adhesive molecules on the inner walls then make it easier for cells to stick and roll along them.

Neutrophils are particularly efficient at rolling and sticking to the inner walls of the blood vessels. They migrate out of the blood vessels in the direction of inflammation,5 and recognize and phagocytize (engulf) pathogens.6 They can release "neutrophil extracellular traps" (NETs), which are sticky extracellular “spider webs” containing microbicidal proteins. NETs act to prevent the spread of infections and kill pathogens.
Current research has revealed that neutrophils also influence other components of the immune system, regulate activities of neighboring cells, and even have a role in "trained immunity," which is a form of "memory" that the innate immune system can have. This is separate from the kind of memory formed by the adaptive immune system.
Eosinophils
Most eosinophils are found in tissues, especially directly underneath barrier tissues like in the gut and respiratory lining. They play a role in defense against invading organisms at these sites, but this role is not well understood. Though they exhibit antibacterial, antifungal, and antiviral effects, they don’t phagocytize (engulf) pathogens as efficiently as neutrophils do.

What you'll typically see in textbooks is that too much eosinophil activity has been associated with asthma and allergy. They’re also known for playing a role in responding to parasites, like worms. More recently, their role in destroying tumor cells, and regulating other immune cell functions (more here), has started to come to light.
Basophils
Basophils are also known for their role in allergic responses. They can release histamine, a compound which contributes to the inflammatory response, like dilation and permeability of blood vessels. They also release substances that allow blood-clotting elements to be delivered to infected areas. They probably play an active role in defense against viruses, including SARS-CoV-2, though it’s not well understood.
Mast cells
Mast cells are similar in both appearance and function to basophils. Like basophils, they can store and release histamine. They’re also known for their role in allergic responses and wound healing, and help recruit other immune cells to sites of infection.
Macrophages, monocytes, and dendritic cells
Next, we’ll cover the cells circled in red below:
Macrophages are white blood cells that are found in most tissues of the body, where they patrol and phagocytize (engulf) pathogens, foreign substances, cancerous cells, and cellular debris. Macrophages that reside in different tissues are sometimes given different names; for example, “microglial cells” are in neural tissues, “Kupfer cells” are in the liver, and alveolar macrophages are in the alveoli of the lungs.
There are several macrophage subsets in the lungs, and they can respond to bacteria, viruses, and allergens; more on that can be found here.

Macrophages are highly plastic and can take various forms. Some express pro-inflammatory molecules (cytokines), recruit other immune cells to sites of infection, and help to maintain their activation. Other types help resolve or wind down inflammation and facilitate tissue repair.
Monocytes are another type of phagocytic white blood cell. There are different subpopulations of monocytes, and they’re often classified by how much they express certain molecular markers, like chemokine receptors.7

“Classical monocytes” mostly circulate in the blood, but can enter into tissues that are infected and differentiate into more inflammatory forms or even macrophages. A smaller proportion of monocytes, “non-classical monocytes,” otherwise known as “patrolling monocytes,” roll along the inner walls of blood vessels (endothelium) instead of circulating freely in the blood (more here). Among other roles, they are thought to survey for injury to the endothelium and remove damaged cells and debris. “Intermediate monocytes” are not well understood but more about their possible roles can be found here.
Monocytes are also highly plastic and can differentiate into macrophages or dendritic cells. Dendritic cells also ingest microbes, but one of their main roles is to process those ingested microbes and present pieces of microbial proteins to cells of the adaptive immune system, so that the adaptive immune system can "learn" from it.8 They also produce molecules like cytokines, which activate other immune cells. Among the cytokines they produce are antiviral cytokines, like type I interferons.
Natural killer cells, other innate lymphoid cells
All the cells we’ve talked about so far are “myeloid cells,” which in the image below are the cells in the shades of pink and purple. Natural killer cells (circled in red) are not part of this group, but are considered lymphocytes, which are the cells in the shades of blue and green:

Among the lymphocytes are B and T cells, which are part of adaptive immunity. Lymphocytes also include other cells that are not shown above, which collectively are called “innate lymphoid cells” or ILCs (more on them here). Natural killer (NK) cells are a type of ILC.
NK cells kill infected, stressed, or abnormal cells, like those found in tumors. NK cells also produce molecules like cytokines, which modulate the behavior of other immune cells.

People with NK cell deficiencies are much more susceptible to viral infections (more here). NK cells likely play an important role against SARS-CoV-2 infection.
NK cells can be found in the blood, and these can migrate to sites of infection. More recently, research has also revealed the presence of tissue-resident NK cells, strategically positioned at sites where they can respond rapidly to infections. These NK cells can be found in many different tissues, like the lungs, gut, uterus, and liver, and vary greatly in function and phenotype depending on the tissues they reside in. More on these tissue-resident cells can be found here, here and here.
NK cells also possess a capacity for “memory” (more here).
Complement
The innate immune system also includes blood serum proteins which together make up the “complement system.” Most of these proteins are synthesized by the liver, but circulate in the blood. In the presence of pathogens, they induce a series of responses that help fight off infection. This includes poking holes in the membranes of pathogens, and attracting and stimulating phagocytic immune cells to clear pathogens.

Complement has a well-established role in immunity against viruses (more here).
The adaptive response depends on the innate response
Adaptive immunity depends on the induction of the innate immune response. That’s because different components of the innate immune response, like the release of certain molecules, like cytokines, are required for full stimulation of the adaptive immune response.
In fact, this is one of the main reasons we have adjuvants in vaccines; adjuvants are molecules that primarily stimulate the innate immune response in order to create the right inflammatory milieu for full elicitation of the adaptive immune response.
Some of the cells of the innate immune system also act as bridges between innate and adaptive immune systems. For example, dendritic cells act as “antigen presenting cells”; they carry9 and “present” microbes or microbial components, to the cells of adaptive immunity so that our adaptive immune system can “learn” from them.
In the final part of this series (Part 4), we’ll review the adaptive immune response.
Though to be clear, B cells, which are part of the adaptive immune system, also have some of these receptors.
These patterns in microbes are called pathogen-associated molecular patterns (PAMPs) and they include bacterial lipopolysaccharide, peptidoglycan, lipoteichoic acids, mannans, bacterial DNA, double-stranded RNA, and glucans. These PAMPs are produced only by microbial pathogens, and not by their hosts. They are usually structures shared by entire classes of pathogens. For example, all gram-negative bacteria have lipopolysaccharides, so a lipopolysaccharide pattern-recognition receptor can detect the presence of virtually any gram-negative bacterium.
I often see papers or textbooks saying that neutrophils are the “first responders” against various infections. It might be that neutrophils are the first to cross the blood vessels to get into infected tissues, but they may not actually be the “first responders,” since there are immune cells that normally reside in tissues, like resident macrophages or natural killer cells. My guess is that those might actually respond before neutrophils, at least some of the time.
This process is called “extravasation.”
They’re also the predominant cells found in pus.
In particular you might see these cells classified according to how much they express the CD14 and CD15 receptors.
Otherwise known as “antigen presentation.”
In many cases they ingest the microbes, break them down, then present pieces of the microbial proteins.





Thank you so much for these explanations with the complex science broken down to elements that help those of us without biology education to begin to grasp the process; it's awesome help!!
Great series. I appreciate your simplified explanations. And those Janeway’s Immunobiology graphics are the best!
Question (for anybody here). I recall reading fairly early on in the C19 pandemic, but after the vax had been rolled out for a while, that secretory IgA was diminished or suppressed in the vaccinated. Anyone have any further info on this, or know of any research? And could this be one of the reasons the vaxxed are becoming the more prone Sars-CoV-2 sickened? 🤔